Home Health Care Eligibility: Your 2026 Guide | Vanika
Learn the home health care eligibility —Medicare rules, homebound criteria, skilled services, and how to apply without the confusion.
Home health care is one of those things that sounds simple—care, at home—until you actually try to figure out eligibility for home health care and realize it comes with rules, forms, and enough acronyms to make you miss high school algebra. Still, when it fits, it’s a game-changer.
Home health care is a vital service that allows individuals to receive medical care in the comfort of their own homes. This guide breaks down the eligibility criteria for home health care so you can understand what typically qualifies, what doesn’t, and what steps to take next. Many people run into barriers when trying to get the services they need—especially older adults, people living with chronic conditions, and families suddenly thrown into “care coordinator” mode (which, let’s be honest, none of us applied for).
If you’re here because you’re trying to keep a loved one safe at home—or you’re recovering yourself and the couch is calling your name—this will walk you through the core requirements, the types of services that qualify, Medicare and Medicaid basics, and what the application process usually looks like.
What Are the Core Criteria for Home Health Care Eligibility?
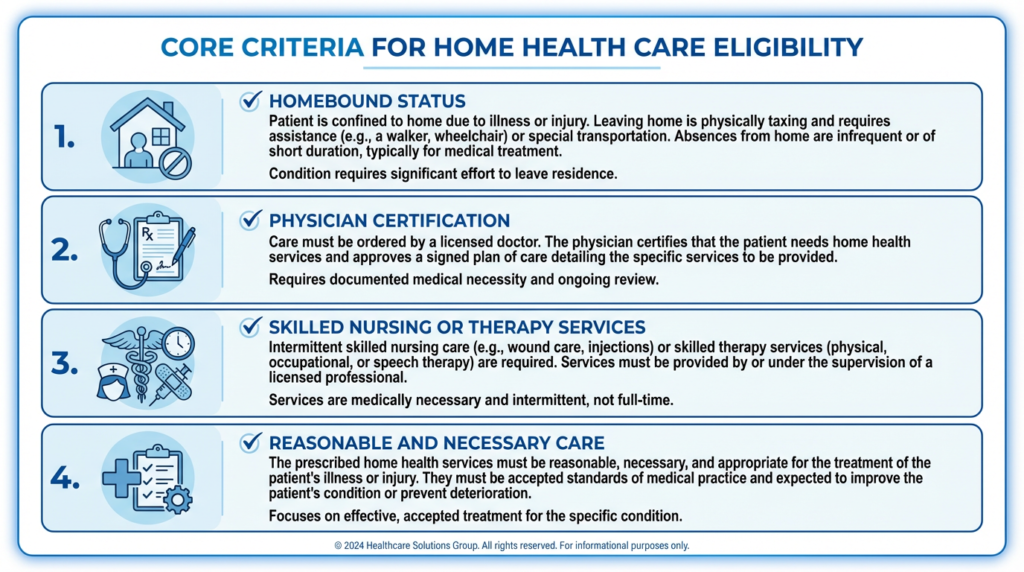
The core eligibility for home health care usually comes down to two big things: (1) a medical need for skilled services and (2) a physician’s order that documents that need. Home health care is designed for people who require medical help but can safely receive that care at home.
In practical terms, qualifying often means you need skilled nursing care (like wound care or medication management) or therapy services (like physical or speech therapy). The key word is skilled—meaning it must be provided by licensed professionals and considered medically necessary.
I like to explain it this way: home health care isn’t “it would be nice to have help.” It’s “a clinician would agree this care needs to happen, and it’s appropriate to do it at home.” That distinction matters because it affects coverage and approvals.
How Does a Physician’s Order and Plan of Care Determine Home Health Care Eligibility?
A physician’s order is the centerpiece of eligibility for home health care. It’s not just a note that says “please help.” It needs to specify:
- Which skilled services are needed (nursing, PT, OT, speech)
- Why they’re needed (the medical condition and goals)
- How often services should be provided
- The overall plan of care
For example, a patient recovering from surgery might require wound care plus physical therapy. Those services need to be clearly included in the physician’s order and plan of care. The plan is also reviewed and updated over time—because healing isn’t a straight line. Some weeks you improve quickly; other weeks your body decides to be dramatic.
Further emphasizing these requirements, official guidelines underscore the necessity of physician certification for Medicare-reimbursable home care services.
Medicare Home Care Eligibility: Physician Certification & Skilled Service Criteria
In order for patients to receive home care that is reimbursable by Medicare, a physician must certify the need for services at home and establish the plan of care. The eligibility criteria for home care remain stringent. Physicians must certify that the patient (1) is homebound, (2) is in need of intermittent skilled nursing care, or physical, speech, or occupational therapy. Eligibility for home care certification: what clinicians should know, 1998
That older (but still widely cited) clinical guidance captures the heart of Medicare’s approach: physician oversight + homebound status + skilled need. If you’re trying to understand eligibility for home health care under Medicare, those are your anchors.
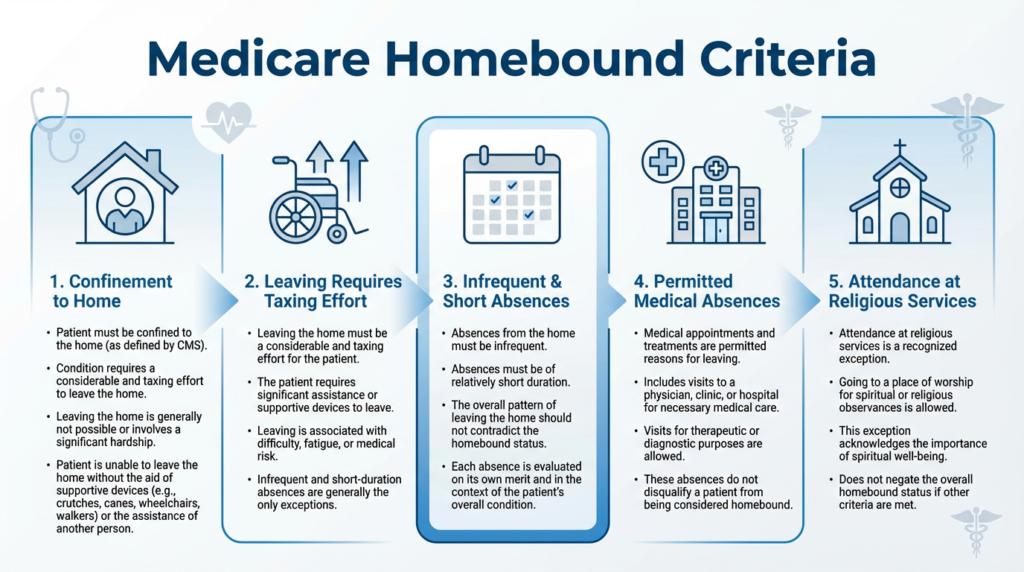
What Is the Medicare Homebound Definition?
Medicare defines “homebound” status as a condition where leaving home is medically contraindicated or it takes a considerable and taxing effort. This definition is central to eligibility for home health care under Medicare.
Here’s what trips people up: “Homebound” doesn’t mean “never leaves the house.” It means leaving home is hard, unsafe, or medically unwise in a consistent way.
To qualify, patients generally must:
- Need help from another person or
- Need a supportive device (walker, wheelchair, crutches) or
- Have a condition that makes leaving home risky
And absences from home should be infrequent or short. Going to medical appointments is fine. A quick outing for something essential is often fine. The point is that the person isn’t realistically able to come and go like usual.
If you’re reading this and thinking, “But my dad goes to dialysis—does that ruin eligibility?” Usually no. Routine medical treatment is one of the common reasons Medicare expects someone might still leave home.
Which Skilled Nursing and Therapy Services Qualify for Home Health Care?
Home health care includes skilled nursing and therapy services that help patients recover, stabilize, and stay as independent as possible. If you’re assessing eligibility for home health care, this is where the “what kind of help” question gets answered.
What Skilled Nursing Care Services Are Covered?
Skilled nursing care under home health typically includes clinical services performed by licensed nurses, such as:
- Wound care and dressing changes
- Medication management and teaching
- Monitoring vital signs and symptoms
- Injections or IV therapy (when ordered)
- Disease management education (e.g., heart failure, diabetes)
Each service has to be medically necessary and documented in the plan of care. In other words, the nurse isn’t just checking in because it’s comforting (though a good nurse can be very comforting). They’re there for skilled medical reasons tied to outcomes.
How Do Physical, Occupational, and Speech Therapies Affect Eligibility?
Therapies are often the reason people qualify for home health, especially after surgery, illness, or a fall.
- Physical therapy (PT) helps with strength, balance, mobility, and safe walking.
- Occupational therapy (OT) focuses on daily living—bathing safely, dressing, cooking, transferring in and out of bed, and adapting the home environment.
- Speech therapy (SLP) addresses communication issues and swallowing difficulties.
Each therapy must be prescribed and included in the plan of care to meet eligibility for home health care criteria. The goal is usually to help someone regain function—or prevent decline—so they can live safely with less intensive care over time.
How Does Medicare Define and Cover Home Health Care Eligibility?
Medicare has detailed guidelines for eligibility for home health care, and those rules often become the “default standard” for many home health agencies—even when the patient isn’t on Medicare. It’s kind of like how airline rules feel universal, even when you’re flying a different airline. Once you know them, you start spotting them everywhere.
Indeed, Medicare’s regulations often serve as a benchmark for home health agency interactions, even for non-Medicare patients, outlining strict eligibility and service requirements.
Medicare Home Health Regulations: Key Eligibility & Service Requirements
Medicare’s regulations are often considered the standard of care for all home health agency interactions, even when a patient does not have Medicare insurance. These regulations require patients who receive home health care services to be under the care of a physician and to be homebound. The patient must have a documented need for skilled nursing care or physical, occupational or speech therapy. The care must be part time (28 hours or less per week, eight hours or less per day) and occur at least every 60 days except in special cases. Home health care, 1998
That “part-time” point matters. Home health is not the same as 24/7 caregiving. If a person needs constant supervision for safety, that’s often a different category of care.
What Are Medicare Part A and Part B Coverage Criteria?
Medicare Part A covers home health care services when patients meet certain criteria—most notably being homebound and needing skilled nursing or therapy services. Medicare Part B can also cover home health services in situations where Part A doesn’t apply, and it may cover outpatient therapy and certain medical supplies.
To qualify under either, patients typically need:
- A physician’s order
- A plan of care
- A documented skilled need
- Homebound status (for Medicare home health benefit)
One of the best things you can do is ask the physician or discharge planner (if you’re coming from a hospital) to clearly document why home is the right setting and what skilled services are needed. Clear documentation reduces delays—because nothing says “fun week” like calling three different offices to get one missing signature.
Which Home Health Care Services Does Medicare Cover and Exclude?
Medicare generally covers:
- Skilled nursing care (intermittent)
- Physical therapy
- Occupational therapy
- Speech therapy
- Medical social services (as part of care)
- Home health aide services when tied to skilled care
Medicare typically excludes:
- Long-term personal care by itself (help bathing, dressing, meal prep) if there’s no skilled care need
- 24-hour home care
- Custodial care as the primary service
This is a common source of confusion. Families hear “home health” and think it includes a daily helper for everything. Sometimes you can get limited aide services as part of a skilled plan—but the anchor remains eligibility for home health care through skilled, medically necessary services.
What Are Medicaid and Private Insurance Eligibility Requirements for Home Health Care?
Medicaid and private insurance can also cover home health services, but their rules may look different. If you’re exploring eligibility for home health care outside Medicare, it helps to treat each payer like its own mini-universe.
How Do Medicaid Home Health Eligibility Rules Vary by State?
Medicaid rules vary because each state administers its own program. In general, Medicaid may cover home health services for people who:
- Meet income and asset thresholds
- Have a documented medical need
- Receive services through approved providers
States also differ in:
- Which services are covered
- Whether there are caps or limits
- What documentation is required
- Whether personal care services are available through waiver programs
If you’re not sure where to start, a good first step is calling your state’s Medicaid office or talking with a hospital social worker. They often know the fastest route through the system (and yes, that’s a real superpower).
What Should You Know About Private Insurance Coverage for In-Home Care?
Private insurance coverage for home health care varies widely. Some plans mirror Medicare rules. Others cover a broader range, and some require prior authorization.
If you’re using private insurance, check:
- Whether the agency must be in-network
- Whether pre-approval is required
- Whether there are visit limits
- What your co-payments or deductible look like
I always recommend asking for the plan’s coverage criteria in writing. Not because we love paperwork (we don’t), but because it prevents “But the rep told me…” arguments later.
How Can You Apply and Qualify for Home Health Care Services?
Applying for home health care usually follows a predictable sequence. The key is to make sure the documentation matches the real clinical need—because eligibility for home health care is often decided on what’s written down, not just what’s true.
What Are the Steps to Apply for Home Health Care?
The process typically looks like this:
- Start with a physician referral (often from a primary care provider, specialist, or hospital discharge team).
- The physician issues an order and establishes the plan of care.
- You choose (or are referred to) a home health agency.
- The agency completes an assessment and coordinates start of care.
A practical tip: if you’re coming home from the hospital, ask the discharge planner to walk you through which agencies serve your area and accept your insurance. That one conversation can save you hours.
What Is the Role of Face-to-Face Evaluation and Certification?
A face-to-face evaluation is a key part of Medicare home health certification. It must occur within 90 days before or 30 days after the start of services. A healthcare provider documents the patient’s condition and confirms the need for home health.
This step matters because it supports the medical necessity behind eligibility for home health care. And yes—if the timing is off or the documentation is incomplete, it can cause delays. It’s annoying, but it’s fixable. If you’re stuck, ask the agency what specific document is missing and which office needs to send it.
Which Medical Conditions and Scenarios Commonly Qualify for Home Health Care?
There’s no official “list” that automatically guarantees eligibility, but certain conditions and scenarios commonly meet eligibility for home health care requirements because they involve skilled needs at home.
How Does Home Health Care Support Chronic Illnesses?
Home health care can be especially helpful for chronic illnesses such as diabetes, heart disease, COPD, and other conditions that require regular monitoring, education, and symptom management.
For example, skilled nursing can help a patient understand medications, monitor warning signs, and reduce preventable complications. Therapy services can build strength and stability, which can lower fall risk—something that matters a lot when someone’s living independently.
One reason this matters: hospital readmissions are stressful and expensive, and home health is often part of a broader strategy to keep people stable at home. If you’ve ever tried to “just rest” while also juggling medications, appointments, and symptoms, you know how quickly things can slide without support.
When Is Home Health Care Appropriate for Post-Surgery and Injury Recovery?
Home health care is commonly used after surgery or injury when patients need skilled support during recovery. This can include:
- Wound care
- Mobility training and strengthening through PT
- OT to regain independence with daily activities
- Medication management and safety checks
If someone is homebound due to recovery and needs skilled services, they may meet eligibility for home health care—especially in the weeks immediately after discharge.
I’ve watched families breathe a visible sigh of relief once a therapist starts coming to the home. Not because therapy is “easy” (it isn’t), but because suddenly there’s a plan, measurable progress, and a professional saying, “Here’s what we’re working on next.” That kind of clarity is underrated.
Conclusion: Making Sense of Eligibility for Home Health Care (Without the Headache)
If you take one thing from this guide, let it be this: eligibility for home health care usually depends on a documented skilled need, physician oversight with a plan of care, and—under Medicare—meeting the homebound definition.
Once those pieces are in place, home health can provide the right level of medical support while letting people heal and manage conditions where they’re most comfortable: at home. And honestly, most of us recover better when we’re sleeping in our own bed, eating our own food, and not listening to hospital hallway announcements at 2 a.m.
If you think you or a loved one might qualify, start with the physician conversation and ask directly: “Do we meet eligibility for home health care? What skilled services would be medically necessary at home?” Those two questions can speed up the process more than you’d expect.
And if the system feels complicated, you’re not imagining it. But with the right documentation and a clear plan, it becomes manageable—and you don’t have to figure it out alone.