Healthy Teeth & Gums: Dental Care Tips & Treatments (2025)
A practical dental care guide for healthier teeth and gums—better brushing, fewer cavities, kid tips, emergencies, and gum disease care.
Dental care is the mix of everyday habits and professional support that keeps your mouth comfortable, your teeth doing their job, and your smile looking like you didn’t just survive a week of coffee, deadlines, and “I’ll floss later” promises. If you’ve ever bought floss with big self-improvement energy and then watched it quietly expire in a drawer… welcome. No judgment. I’ve been there.
This guide pulls together what actually matters—prevention strategies, common treatment options, kid routines, emergency “what do I do right now?” steps, and periodontal care—so you can protect enamel, gums, and overall oral health without feeling like you need to memorize the dental aisle.
A lot of people deal with plaque buildup, tooth decay, sensitive gums, and the ever-haunting question: “Is this urgent, or can I ignore it until my next cleaning?” (Sometimes you can. Sometimes your tooth will respond by waking you up at 2 a.m. like it’s paid by the hour.) The goal here is simple: give you clear, evidence-based steps that make dental care feel doable, not dramatic.
How Can an Electric Toothbrush Improve Gum Health?
An electric toothbrush can improve gum health because its rapid oscillating or sonic movements disrupt plaque biofilm more efficiently than most manual brushing—especially at the gumline where gingivitis likes to quietly set up camp. The key isn’t that electric brushes are fancy. It’s that they’re consistent. They do the repetitive motion for you, so your job is positioning and coverage, not scrubbing like you’re trying to remove permanent marker from a wall.
If you want a credible, non-marketing reference: a well-known Cochrane review (2014) found powered toothbrushes reduce plaque and gingivitis more than manual brushes, with oscillating-rotating brushes showing a clear advantage in many comparisons. Translation: there’s real evidence behind the upgrade.
Two features matter a lot for gum health:
- High-frequency motion: more plaque disruption with less aggressive hand pressure.
- Pressure control: sensors (or braking systems) that stop you from going full “power washer” on your gums.
Using an electric brush with soft bristles and a built-in timer nudges you into the recommended two-minute routine. I used to swear I brushed for two minutes. Then I got a timer and discovered my “two minutes” was more like 50 seconds plus confidence. The timer didn’t just improve my brushing—it exposed my optimism.
Electric toothbrush benefits for gum health include plaque reduction, pressure feedback, and easier technique control, which together reduce gum trauma and help slow gum disease progression. Next, let’s talk sensitive gums—because if brushing hurts, you’re not going to do it well (or consistently), and dental care turns into a chore you avoid.
What Are the Benefits of Using an Electric Toothbrush for Sensitive Gums?
Electric toothbrushes can be especially helpful for sensitive gums because they combine gentle cleaning with built-in guardrails. Instead of relying on willpower (“be gentle, be gentle…”) you get tools that guide your behavior—kind of like bumpers in bowling, but for your gumline.
What helps most:
- Soft brush heads: less abrasion at the gumline.
- Pressure sensors: a literal reminder to lighten up.
- Gentle/low-power modes: great if you’re dealing with inflammation or recession.
- Timers and quadrant pacing: keeps you from spending 90% of your time on the front teeth and forgetting the molars exist.
Clinical comparisons generally show modest but consistent improvements in plaque removal and gingival health for electric brush users—especially when people actually use the timer and pressure features. In other words: the brush helps most when it changes your routine, not just your shopping cart.
If you have root sensitivity or exposed dentin, pair your electric brush with a desensitizing toothpaste (potassium nitrate or stannous fluoride are common) and avoid aggressive “sawing” motions. Let the brush do the work. Your gums are not a cast-iron pan that needs extra scrubbing.
How to Choose the Best Electric Toothbrush for Gum Health?
Choosing the best electric toothbrush for gum health comes down to three practical criteria: gentle bristles, pressure management, and a motion type you’ll actually tolerate every day. Because the best brush is the one you’ll use twice a day without negotiating with yourself like it’s a hostage situation.
- Brush head design (soft matters): Soft or extra-soft bristles minimize gingival abrasion. If your bristles flare quickly, you’re probably pressing too hard.
- Pressure sensor (big deal for many people): If you’ve had gum recession, sensitivity, or you know you’re a “hard brusher,” this is worth prioritizing.
- Motion type:
- Sonic brushes use high-frequency vibration and fluid dynamics to disrupt plaque beyond direct contact.
- Oscillating-rotating brushes use a small round head that mechanically cleans at the margins.
Pick what feels comfortable. Some people love sonic; others feel like it’s tickling their skull (which is… an experience). Comfort matters because dental care is repetitive—like dishes—so your setup needs to be sustainable.
Also consider battery life, replacement-head cost, and ADA acceptance when available. Replace brush heads every three months (or sooner if they look like they’ve been through a wind tunnel). And if you’re thinking, “But mine still works”—sure, so does a frayed mop.
To clarify differences between electric and manual brushes, the following comparison highlights mechanisms, plaque-effectiveness, and suitability for sensitive gums.
Different brush types compare across mechanism, effectiveness, and suitability.
| Brush Type | Mechanism | Effectiveness for Plaque Removal | Suitability for Sensitive Gums |
|---|---|---|---|
| Sonic Electric | High-frequency vibrations create fluid dynamics | High — disrupts biofilm beyond bristle contact | Very suitable with soft heads and low-power modes |
| Oscillating-Rotating Electric | Rotating/oscillating head mechanically removes plaque | High — excellent at subgingival margin cleaning | Suitable when pressure control present |
| Manual (Soft bristle) | Manual back-and-forth motion | Moderate — technique-dependent | Acceptable if gentle technique used and user disciplined |
This table summarizes how different toothbrush types act on plaque and which are best for sensitive gums, aiding your selection process before moving to cavity prevention strategies.
What Are the Most Effective Cavity Prevention Tips?

Cavity prevention isn’t about having “perfect teeth.” It’s about reducing how often your enamel gets hit with acid—and then giving it the tools (fluoride, saliva, time) to recover. That’s the real rhythm of good dental care.
The core pillars are mechanical plaque control, fluoride-mediated remineralization, dietary management (especially snacking frequency), and professional preventive treatments.
Brush twice daily with fluoride toothpaste, clean between teeth daily, limit frequent sugar/acid exposure, and show up for routine cleanings. Fluoride helps enamel remineralize and become less soluble in acid. Sealants act like little raincoats for molar grooves—especially helpful for kids and teens.
Below is a concise, actionable checklist of high-impact cavity prevention steps you can implement immediately.
Effective cavity prevention uses these five steps:
- Brush twice daily with fluoride toothpaste for two minutes to promote remineralization.
- Clean interdental spaces once daily with floss or interdental brushes to remove plaque.
- Reduce frequent snacking on sugary foods and acidic drinks to limit enamel acid exposure.
- Use fluoride treatments as indicated by risk (toothpaste, varnish, or in-office applications).
- Consider dental sealants for molars and maintain routine professional exams and cleanings.
These practical steps reduce decay risk by targeting enamel demineralization and plaque accumulation; next, we compare preventive measures in more detail to show their mechanisms and recommended use.
To compare prevention options and their evidence, the table below summarizes mechanisms, effectiveness, recommended ages, and evidence level.
| Preventive Measure | Mechanism | Recommended Age/Use | Evidence Level |
|---|---|---|---|
| Fluoride (toothpaste/varnish) | Enhances enamel remineralization | All ages; varnish for high-risk children/adults | High |
| Dental Sealants | Barrier over pits and fissures | Children/adolescents with erupted molars | High |
| Dietary Counseling | Reduces fermentable carbohydrate exposure | All ages; focus on frequent snackers | Moderate |
| Interdental Cleaning | Removes plaque from contact areas | From floss-introduction age onward | High |
This comparison clarifies which interventions suit different age groups and risk profiles, supporting personalized prevention planning and leading naturally into daily habit specifics that parents and adults should adopt.
Which Daily Habits Help Prevent Tooth Decay and Cavities?
Daily habits that prevent decay are the “boring basics” done well—plus a couple of smart tweaks that save your enamel from constant repair mode. You’re aiming to reduce acid attacks, boost remineralization, and keep plaque from settling in like it pays rent.
Brush twice daily for two minutes with fluoride toothpaste. Clean between teeth daily (floss, picks, or interdental brushes—choose your tool, not your excuse). Avoid sipping sugary drinks between meals, because frequent exposure keeps enamel under attack even if you “don’t drink that much.”
Saliva is your mouth’s built-in defense system. It buffers acids, clears food debris, and helps remineralize enamel. So supporting salivary flow is quietly one of the best dental care moves you can make. Staying hydrated helps. Chewing sugar-free xylitol gum after meals can help some people too—especially if you’re prone to dry mouth or you snack a lot. (Also, it gives you something to do besides scrolling.)
Habit formation matters more than motivation. Put floss somewhere visible. Use a timer. Keep a spare toothbrush where you’ll actually use it. Little systems beat big promises—every time.
These habit-based steps tie into professional treatments like fluoride varnishes and sealants, which provide added protection based on individual decay risk and age.
How Do Fluoride and Dental Sealants Protect Teeth from Cavities?
Fluoride and dental sealants protect teeth in different ways, and they work best as a team.
Fluoride strengthens enamel and supports repair of early damage. Public health organizations like the CDC have long highlighted fluoridation and fluoride toothpaste as major contributors to reduced tooth decay at the population level.
Sealants protect chewing surfaces of molars by physically blocking pits and fissures where plaque gets trapped. They’re especially valuable for kids and teens with newly erupted molars, but adults with deep grooves or a history of occlusal decay can benefit too.
Both strategies are supported by strong clinical evidence and are typically guided by a caries risk assessment during dental visits.
How Should Children Practice Proper Oral Hygiene?
Kids’ dental care is its own universe, mostly because children have the attention span of a hummingbird that just discovered cupcakes. The good news: you don’t need perfection. You need consistency, age-appropriate routines, and a tiny bit of creativity.
Children’s oral hygiene should follow milestones: gum wiping in infancy, supervised brushing with fluoride toothpaste in toddler years, and gradually increasing independence with brushing and flossing in school-age years. The earlier the routine becomes “normal,” the fewer battles you’ll fight later.
The next subsections provide clear, practical routines for different age groups and explain when to schedule the initial dental visit to maximize preventive benefit.
What Are the Best Oral Hygiene Practices for Kids?
Oral hygiene for children follows a simple progression tied to development: infants need gum wiping, toddlers transition to fluoride toothpaste with caregiver brushing, and school-aged children brush twice daily and begin flossing when teeth touch.
Use a smear (rice-sized) for children under 3 and a pea-sized amount from ages 3–6. Supervise brushing until your child has good dexterity, often around age 7–8. (A practical test: if they can’t reliably tie their shoes, they probably need brushing backup.)
Introduce flossing when teeth touch and consider dental sealants for permanent molars when they erupt. Positive reinforcement—routine timing, a fun timer, a sticker chart, letting them pick the toothbrush—makes habits stick.
These routine practices naturally connect to scheduling the first dental visit early, which the next section addresses.
When Should Children Have Their First Dental Visit?
Children should have their first dental visit by the eruption of the first tooth or by their first birthday, whichever comes first. This guideline is widely recommended by pediatric dental organizations because early visits focus on prevention and parent coaching, not scary procedures.

Early appointments often include a gentle exam, brushing demonstrations, fluoride guidance, and feeding/snacking tips that affect decay risk. It also helps normalize the dental office so it feels like a routine stop—not a place you only go when something hurts.
Scheduling this initial visit establishes a preventive partnership and reduces the likelihood of advanced decay later, which transitions into when urgent dental treatment becomes necessary.
When Is Urgent Dental Treatment Necessary?
Urgent dental treatment is necessary when symptoms suggest immediate risk: severe, unrelenting pain; uncontrolled bleeding; rapidly spreading swelling; fever with oral infection signs; or trauma like a knocked-out tooth.
If you’re ever unsure, here’s my rule of thumb: if you’re thinking, “This is getting worse fast,” treat it like urgent. Dental infections can spread, and facial swelling isn’t a “wait and see” situation.
Immediate self-care steps can stabilize things until you get professional help: control bleeding with gauze and firm pressure, use cold compresses for swelling, and preserve an avulsed tooth in milk or saline (keep it moist).
Knowing which symptoms constitute an emergency—and what to do first—reduces delays and improves outcomes.
What Are Common Dental Emergencies and How Should They Be Managed?
Common dental emergencies include avulsed (knocked-out) teeth, fractured teeth, acute infections (abscesses), and uncontrolled oral bleeding.
For an avulsed permanent tooth, immediate reimplantation or transport in milk/saline improves the chance of saving it; if reimplantation isn’t possible, keep it moist and seek urgent care quickly.
Cracked or fractured teeth should be protected from further damage, rinsed gently, and managed for pain control until repaired; large fractures may expose pulp and require prompt attention.
Signs of an abscess—localized swelling, fever, severe throbbing pain, or spreading facial swelling—often require urgent drainage, antibiotics when indicated, and definitive dental treatment to prevent complications.
These first-aid steps inform triage decisions and lead naturally to how to locate emergency services rapidly.
How to Find and Access Emergency Dental Services Quickly?
When you need emergency dental care, speed comes from being prepared and describing symptoms clearly.
Use search phrases like “24-hour dentist,” “emergency dentist,” or “urgent dental clinic.” Before you call, jot down age, symptoms and timing, fever/swelling presence, trauma details, and take photos if relevant. You’re not being dramatic—you’re being efficient.
If teledentistry is available, it can speed up triage. For severe systemic symptoms—high fever, uncontrolled bleeding, difficulty breathing or swallowing—an emergency department may be necessary. For many tooth-related emergencies, a dental urgent care clinic or on-call dentist can provide faster, dentistry-specific treatment.
These access strategies set up the final major topic: recognizing and treating periodontal disease, which often requires staged intervention.
What Are the Symptoms and Treatments of Periodontal Disease?
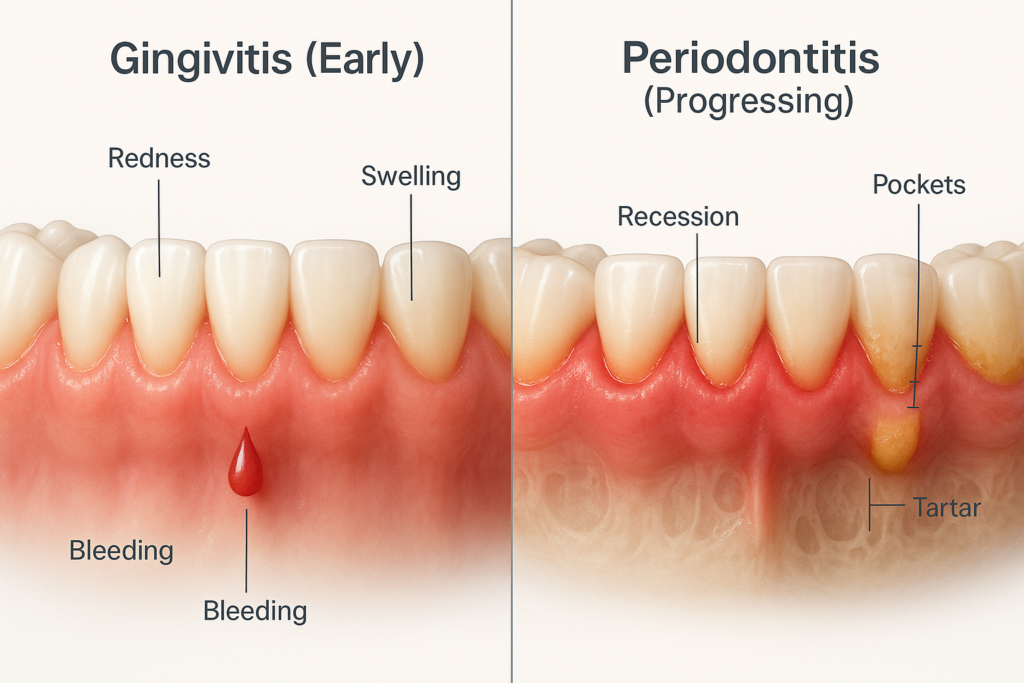
Periodontal disease ranges from reversible gingivitis to periodontitis, where the supporting bone and connective tissue are damaged. It’s driven by plaque-induced inflammation that doesn’t stay “just on the gums” if it’s ignored.
Early signs include redness, swelling, and bleeding when brushing or flossing. Later signs include gum recession, deeper pockets, tooth mobility, and bite changes. Diagnosis is based on clinical exam and periodontal probing (plus X-rays when needed).
Treatment follows a stepped approach: improved home care and professional scaling first, then deeper therapy like scaling and root planing, and sometimes surgery for advanced cases.
Addressing periodontal disease early—paired with consistent dental care habits—can stop progression and preserve teeth.
The following subsections help you recognize early signs and outline available treatments, including when specialist care is indicated.
How to Recognize Early Signs of Gingivitis and Periodontitis?
Recognizing early signs includes bleeding during brushing or flossing, persistent bad breath, swollen or tender gums, and gum recession.
Gingivitis often presents with reversible inflammation and bleeding without attachment loss. Periodontitis shows deeper pockets, bone loss on radiographs, and sometimes tooth mobility.
Regular self-checks—watching for bleeding, changes in gum color/contour, and looseness—should prompt scheduling a professional periodontal evaluation. If bleeding is consistent, don’t shrug it off. Bleeding is information.
To summarize stages and recommended interventions, the table below outlines disease stage, symptoms, common treatments, and typical follow-up.
| Stage | Common Symptoms | Typical Interventions | Follow-up |
|---|---|---|---|
| Gingivitis | Bleeding, redness, swelling | Improved home care, professional cleaning | Re-evaluate 4–12 weeks |
| Mild–Moderate Periodontitis | Pocketing, early bone loss | Scaling and root planing, localized antimicrobials | Periodontal maintenance every 3–4 months |
| Advanced Periodontitis | Tooth mobility, significant bone loss | Periodontal surgery, regenerative procedures | Specialist follow-up and maintenance |
This summary clarifies the escalation from hygiene-focused care to specialist interventions and prepares readers to understand specific procedures and maintenance needs.
What Are the Available Treatments for Periodontal Disease?
Treatment typically begins with non-surgical therapy: scaling and root planing under local anesthesia plus improved home care. The goal is to remove subgingival calculus and disrupt biofilm so inflamed tissue can heal.
Adjunctive options (for select cases) include localized antimicrobials in pockets, systemic antibiotics when indicated, and risk-factor management (smoking cessation, diabetes control, and lifestyle factors that influence inflammation).
When non-surgical measures aren’t enough—especially with deeper pockets or certain bone defects—surgical options like flap surgery, guided tissue regeneration, or bone grafting may be recommended.
Long-term success depends on maintenance: periodontal maintenance visits every three to four months and consistent home dental care habits.
Each procedure targets specific pathological features and is selected based on severity, which underscores the importance of regular monitoring and personalized planning.
Early detection and routine cleaning: Prevents disease progression through plaque control.
Scaling and root planing: Removes subgingival calculus and disrupts biofilm to allow healing.
Surgical regeneration: Restores lost supporting structures when indicated.
These treatment steps demonstrate a tiered approach to managing periodontal disease and emphasize the partnership between patient home care and professional therapy.
Monitor bleeding and gum changes: Schedule evaluation if symptoms persist.
Adopt rigorous oral hygiene: Effective brushing and interdental cleaning are foundational.
Commit to maintenance: Regular periodontal maintenance reduces relapse risk.
Conclusion
Maintaining strong dental care habits is one of those “small effort, big payoff” life upgrades. You don’t need to be perfect—you need to be consistent. Brush well, clean between teeth, keep sugar exposures reasonable, use fluoride, and show up for professional visits before small problems become expensive surprises.
If I could go back and give my younger self one piece of advice, it would be this: treat your gums like they matter (because they do), and don’t wait for pain to start caring. Most major issues—cavities, gum disease, even sensitivity—start quietly.
With prevention, early intervention, and personalized treatment when needed, you can protect your teeth, support gum health, and keep your mouth feeling good for decades. And honestly? A mouth that doesn’t cause drama is an underrated luxury.






2 Comments
Comments are closed.