Mental Health: How Society Plays a Role (Vanika)
Let us walk through how society affects mental health—what pushes people toward burnout, anxiety, depression, and distress, and what actually helps.
When people talk about mental health, it often gets framed as something individual:
Fix your mindset. Sleep more. Meditate. Be grateful.
Sure, those things can help. But if you’ve ever tried all the “right” things and still felt overwhelmed, anxious, numb, or just done, you’ve probably run into a bigger truth: mental health doesn’t exist in a vacuum. It lives inside real lives, real neighborhoods, real systems.
Society affects mental health in ways that are easy to overlook because they’re so normal we treat them as “just life.” Things like:
- Trying to stay calm when your rent keeps going up but your pay doesn’t.
- Feeling unsafe in your own neighborhood.
- Growing up in a culture where you’re supposed to “be strong” instead of asking for help.
- Sitting on a waitlist for a therapist for months while you’re barely holding it together.
I’ve heard so many versions of the same sentence: “I feel like I should be coping better than this.” And I always want to respond, “You’re not broken. You’re just living in a world that demands a lot and gives very uneven support in return.”
Here’s the thing: Mental health challenges exist, whether you like it or not. You’re not imagining it. The world around you really does matter and the society you’re in influence mental health more than you thought it should.
Society and Mental Health Problems
When we ask how society affects mental health, we’re really asking:
How much of what I’m feeling is “just me,” and how much is a normal reaction to a tough environment?
A lot of us were trained to think it’s mostly “just you.” If you’re struggling, the usual script is:
- You’re not trying hard enough.
- You’re too sensitive.
- You need better habits.
- You should “focus on the positive.”
There’s a place for personal responsibility. But it’s not the whole story, and honestly, it’s not even the first chapter for many people.
Think of it like a garden. Your genetics and personal history are the seeds. Some seeds really are more sensitive. Some are sturdy no matter what. But the soil, the weather, the water, the pollution, the person (or lack of person) tending the garden—that’s society.
You can do everything “right” as a seed. But if the soil is dry or toxic, the weather is extreme, and people keep stomping through the garden on their way to somewhere else, you’re going to struggle. That doesn’t mean you’re weak. It means the conditions are harsh.
When we look at how society affects mental health, we’re paying attention to questions like:
- Can you realistically cover food, housing, and bills, or is every month a mini emergency?
- Do you feel safe walking in your own neighborhood, or are you constantly on alert?
- Does your culture make it okay to say, “I’m not okay,” or does it quietly punish that honesty?
- Do you feel like you belong anywhere, or are you always on the outside looking in?
Once you start seeing these patterns, your internal monologue begins to shift. Instead of “What’s wrong with me?” it becomes “Look what I’ve been trying to carry with very little support.”
That shift matters. It doesn’t erase the pain. But it replaces shame with context—and that’s a healthier starting point for any kind of healing.
Protective Factors: The Social Drivers That Influence Mental Health
There are many ways society affects mental health, but a few forces show up again and again. They’re like the background settings of everyday life: money, housing, community, culture, access to care, and systemic inequality.
These don’t show up as bullet points in real life. They show up as:
- The late-night money panic.
- The quiet ache of loneliness.
- The awkward silence when you open up about mental health and everyone changes the subject.
- The 10th unanswered voicemail to a therapist’s office.
Let’s break these drivers down.
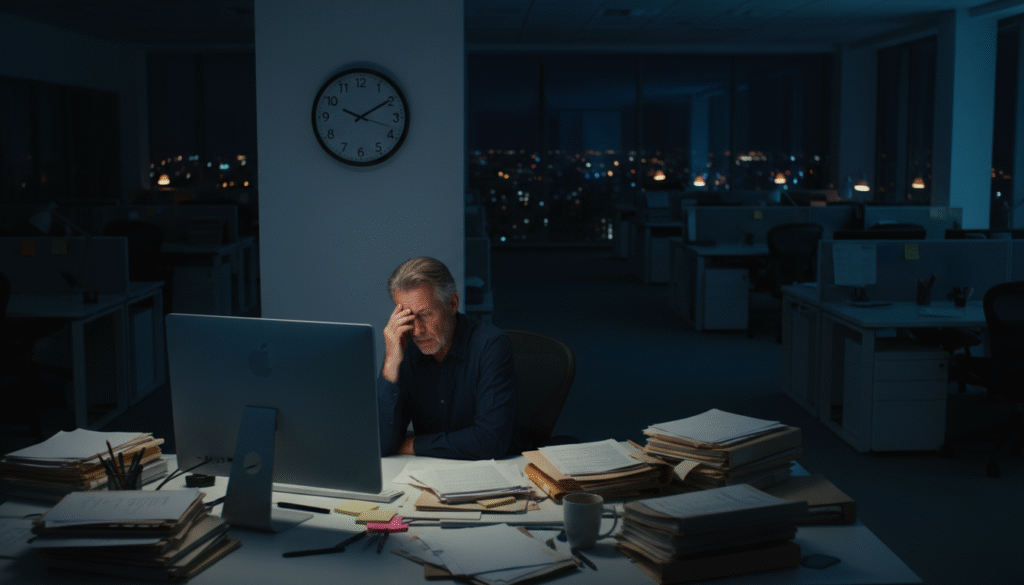
1. Economic Factors: Poverty and Housing Insecurity
It’s almost funny how often we try to talk about mental health without talking about money.
Money doesn’t buy happiness, but it absolutely buys options: food that isn’t the cheapest thing on the shelf, a stable place to live, time off when you’re sick, child care, transportation, medication, therapy. It buys breathing room—and breathing room is incredibly soothing to your nervous system.
Living in poverty isn’t just “having less.” It’s living in constant mental arithmetic:
- “If I pay this bill, I can’t pay that one.”
- “If the car breaks down, I’m done.”
- “If I miss one paycheck, I’m in serious trouble.”
I remember hearing someone joke, “My therapist told me to reduce my stress and I said, ‘Okay, can you please talk to my landlord and my boss?’” It was a joke, but it landed because it was so close to the truth.
Research backs this up. Studies in journals like the American Journal of Psychiatry have found that people living in poverty are at much higher risk for depression and anxiety. Not because they’re less grateful or less motivated, but because life is a never-ending series of high-stakes decisions.
Housing insecurity pushes this even further. If you’ve ever:
- Moved multiple times in a year because of rising rent,
- Couch-surfed with friends or family because you had no other option,
- Watched your housing costs go up while your income stayed the same,
then you know how quickly “Where will I sleep?” takes over your brain. It’s incredibly hard to focus on self-care or growth when the basics aren’t stable.
This is one of the clearest ways to see how society affects mental health: when people are constantly juggling survival-level problems, their mental health is going to take a hit.
2. Social Isolation and Community Support
Even if you love your alone time (I do), there’s a big difference between choosing solitude and feeling alone in the world.
When you have people you can text at 1 a.m., or someone who notices when you haven’t been yourself, it acts like a cushion for your mental health. The hard stuff still hurts, but it doesn’t feel quite as bottomless.
Now imagine the opposite. Maybe you:
- Moved to a new city.
- Work long, weird hours.
- Have friends online but few nearby.
Your life might look “fine” on the outside: you go to work, you run errands, you nod at people, you make small talk. But sometime on a random evening, it hits you: if something truly went wrong, you’re not totally sure who you’d call.
That realization alone can drop your mood.
Loneliness isn’t just “sadness with extra steps.” A major analysis from Brigham Young University compared loneliness and social isolation to smoking about 15 cigarettes a day in terms of health risk. Fifteen. That’s how deeply wired we are for connection.
On the flip side, I’ve seen what happens when community actually shows up. Neighbors checking on each other. People dropping off meals. Group chats that are more than memes—they’re “Hey, how are you really?”
When we ask how society affects mental health, this is a huge piece of it: are we building cultures where people know and support each other, or are we all quietly drowning in separate corners?
3. Cultural Norms and Stigma Around Mental Illness
Culture is the invisible script we absorb without realizing it.
It tells us what’s “normal,” what’s “dramatic,” what’s “strong,” and what’s “weak.” And when it comes to mental health, those scripts can be either incredibly supportive or incredibly harmful.
In some communities, saying “I see a therapist” is almost trendy—it’s treated like saying you go to the gym. In other communities, that same sentence would land like a confession.
You might have grown up hearing things like:
- “We don’t talk about that outside this house.”
- “You’re fine. Other people have it worse.”
- “Be strong. Don’t make a scene.”
On the surface, that can look like discipline or resilience. But underneath, it often teaches you to swallow your pain, hide your emotions, and pretend you’re okay when you’re not.
I grew up with some of that messaging too: you keep it together, you don’t “burden” people. You show up, no matter what. From the outside, you look functional—even impressive. Inside, you might feel like you’re quietly disappearing.
Stigma isn’t always someone loudly saying, “Therapy is bad.” It’s often more subtle:
- The silence after you open up.
- The quick subject change.
- The “You’re strong, you’ll be fine” that shuts the conversation down.
Over time, this teaches you that being honest about your mental health is risky. So you learn to edit yourself.
Understanding how society affects mental health means recognizing that culture can either make healing easier or block it at every turn.
4. Access to Mental Health Services and Health Care
Let’s say you’ve done the hard part: you admitted you’re struggling and decided you want help. That alone can take months or years.
Now you enter a new maze: actually getting care.
Very quickly, how society affects mental health becomes a logistics problem:
- Do you have health insurance?
- Does your plan cover mental health in a real way—or basically not at all?
- Can you find a provider taking new patients?
- Can you see them without missing work or losing pay?
- Do they understand your culture, language, or background—or will you spend half the session explaining the basics of your life?
I’ve personally been through the “call, voicemail, email, wait” loop looking for a therapist. At one point, I had a mini spreadsheet just to track who I’d contacted, who was full, who didn’t take my insurance, and who never replied. By the time I finally got an appointment, I was already emotionally drained from the process.
Many people never even make it that far.
Agencies like the Substance Abuse and Mental Health Services Administration have been saying it for years: without affordable, culturally competent, and accessible mental health care, the gaps in who gets help and who doesn’t will keep widening.
Access isn’t a luxury feature. It’s the bridge between “I’m struggling” and “I’m getting real support.”

5. Racism, Discrimination, and Social Inequities
There’s no honest way to talk about how society affects a person’s mental health, even emotional well being, without talking about racism, discrimination, and inequality.
Experiencing discrimination—because of race, ethnicity, gender, sexuality, disability, religion, immigration status, or anything else—isn’t just “offensive.” It’s draining in a deep, ongoing way.
It can look like:
- Wondering if you’ll be followed around a store.
- Bracing yourself for “jokes” at work.
- Being talked over or dismissed in medical settings.
- Watching people act surprised that you’re “so articulate” or “so professional.”
One review in JAMA Psychiatry found that perceived discrimination is consistently associated with higher levels of depression, anxiety, and overall psychological distress.
And discrimination isn’t just about one rude comment. It’s also about systems and history:
- Which neighborhoods were historically denied loans and investment.
- Who is more likely to be stopped by police.
- Which schools have fewer resources.
- Who is more likely to be underpaid or not hired at all.
All of that shapes daily stress.
Friends and colleagues have described what it feels like to be the “only one” in a room—whether that’s the only Black person, the only queer person, the only person with a disability, the only immigrant. On the outside, they might seem confident and composed. On the inside, they’re tracking every comment, every look, every shift in tone.
That constant self-monitoring takes a toll on mental health.
So when we say society affects mental health, this is a big part of what we mean: life is simply heavier for some people because of systems they didn’t create but still have to survive.
How Mental Health Challenges Manifest in Society
Once you start to notice how society affects mental health in the background, you also start seeing how it shows up in the foreground—in doctor’s offices, schools, workplaces, families, and your own head.
Mental Health Conditions and Disorders
Some struggles fit neatly into diagnostic labels like major depression, anxiety disorders, bipolar disorder, PTSD, or schizophrenia. Mental health professionals use tools like the Diagnostic and Statistical Manual (DSM) to categorize and treat these conditions.
Society doesn’t single-handedly create every disorder. But it does affect:
- who is more likely to develop certain conditions,
- when symptoms show up,
- how intense they become,
- and who actually gets treatment.
If you grow up dealing with chronic stress—poverty, unstable housing, unsafe environments, discrimination, family conflict—you’re starting life with a heavier emotional load. That load interacts with your biology and experiences.
Later, if you try to get help and run into waitlists, high costs, or providers who don’t get your reality, symptoms can worsen.
So while your mental health isn’t only “about society,” it also isn’t separate from it.
Substance Use Disorders
Substance use and mental health are often tangled together.
For many people, substances start out as a coping tool:
- A drink to calm down after a brutal shift.
- Something to help you sleep when your brain won’t shut off.
- Something stronger to numb memories or pain.
At first, it might feel like it “works.” You get a few hours of relief, a break from constant fear or sadness.
But over time, substance use can turn into a disorder that brings its own problems: health issues, relationship strain, lost jobs, legal trouble—on top of the pain that was already there.
Zoom out further and you can see whole communities hit by waves of substance use issues, often in places with:
- job loss or unstable work,
- poor access to health care,
- generational trauma,
- and very few safe, affordable ways to cope.
Seeing how society could possible contribute to poor mental health doesn’t excuse harmful behavior, but it does challenge the idea that people are just “making bad choices.” Often, they’re trying to cope with overwhelming stress using the tools they have—even if those tools are risky for their mental and physical health.
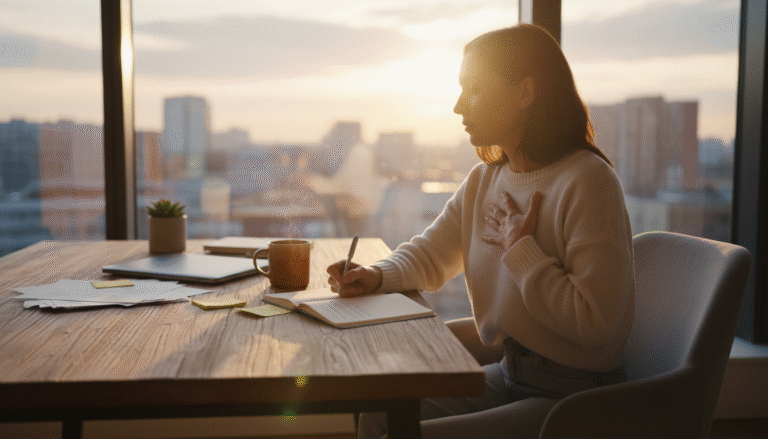
Emotional Distress and Psychological Struggles
Not everyone has—or wants—a formal diagnosis, but that doesn’t mean they’re okay.
There’s a huge group of people walking around with what you could call “everyday distress:”
- Burnout that no weekend can fix.
- A low-level sadness that never fully lifts.
- Anxiety that keeps you in a constant state of “What if?”
From the outside, these people might look completely functional. They show up to work. They smile in photos. They answer emails. But inside, they feel worn down and disconnected from themselves.
A lot of this distress is tied to how society is set up:
- Long work hours with little rest.
- Rising costs and stagnant wages.
- Pressure to always be “on” and productive.
- Social media comparison loops.
- Lack of real downtime or community support.
It’s not that “life is just hard.” It’s that life has been organized in ways that are hard on human nervous systems.
That’s another way society affects mental health—not just through extreme crises, but through a constant drip of stress that slowly adds up.
The Role of Public Health in Addressing Mental Health
For a long time, mental health was framed as an individual problem with individual solutions: you, your therapist (if you could find one), your medication (if you could afford it), your coping skills.
Public health adds a different lens. It asks questions like:
- What patterns do we see across whole communities?
- Who is struggling the most, and what do their lives have in common?
- What can we change about the environment so fewer people end up in crisis in the first place?
Instead of only focusing on treatment after people are already struggling, public health tries to shift some attention to prevention and systems.

Prevention Strategies
Most mental health systems are set up to react—somebody hits a breaking point, and then the system scrambles.
Prevention asks: What if we made it less likely for people to reach that breaking point at all?
That can look like:
- policies that reduce poverty and housing instability,
- workplaces that take burnout seriously instead of glorifying it,
- schools that prioritize emotional learning and address bullying for real,
- trauma-informed care in hospitals, shelters, and social services.
If we go back to the garden metaphor, prevention is about improving the soil and weather instead of waiting until every plant is sick.
Improving Access
Public health also focuses on making support easier to reach.
That might include:
- mental health screenings at regular doctor visits,
- counseling available in schools, colleges, and community centers,
- telehealth options that work even for people without perfect internet or privacy,
- training community health workers and peers to provide basic support.
The goal isn’t to turn every person into a therapist. It’s to make sure help isn’t hidden behind a hundred barriers.
Education and Awareness
Public health campaigns try to change the way we talk about mental health.
When respected people—athletes, artists, community leaders, or just someone in your circle—say, “I deal with anxiety,” or “Therapy helped me,” it quietly rewrites the script.
I’ve watched rooms soften when someone says, “Hey, I’ve been there too.” It doesn’t fix everything, but it takes away some of the loneliness.
Good education doesn’t just list symptoms; it shows people what support can look like and reminds them that struggling doesn’t make them weak or broken.
Research
Finally, there’s the research side—asking what actually helps beyond guesses and good intentions.
Researchers look at things like:
- What happens to mental health when people move into stable, affordable housing?
- How do anti-discrimination laws impact stress in targeted communities?
- Which school or workplace programs actually reduce anxiety, bullying, or burnout?
This kind of research turns “We hope this helps” into “We have evidence this helps,” which can shape laws, budgets, and community programs.
What Can We Do to Improve Mental Health at a Societal Level?
Reading about mental disorders can feel heavy. You might be thinking, “Okay, this makes sense, but I’m one person. I don’t control housing policy or health care.”
That’s true. None of us can fix everything alone.
But change happens at different levels—personal, relational, community, and policy.
You don’t have to do everything. You just have to do something real in your corner of the world.
1. Promote Equitable Access to Mental Health Care
First, we can stop treating mental health care like a luxury for people with extra time and money.
On a larger scale, that might look like supporting:
- policies that expand insurance coverage for therapy and medication,
- funding for community clinics and crisis centers,
- training more diverse mental health professionals,
- programs that bring mental health support into schools, workplaces, and faith communities.
On a personal level, it might mean:
- learning what hotlines, clinics, and resources exist in your area,
- sharing those resources when someone opens up to you,
- supporting organizations that make care more accessible.
2. Reduce Stigma and Normalize Mental Health Conversations
People with mental health issues experience stigma more often than we could imagine; but a lot of stigma melts away when regular people talk honestly.
You don’t have to tell everyone everything. But when it feels safe, you might:
- mention therapy the same way you’d mention a dentist appointment,
- take someone seriously when they say they’re struggling,
- avoid using words like “crazy” as a joke,
- ask, “How’s your mental health lately?” and then really listen.
Sometimes one honest conversation with a friend does more than a whole campaign. When someone you trust says, “Yeah, I’ve had panic attacks too,” or “I’ve been depressed before,” suddenly you’re not a strange exception—you’re human.
3. Address Social Determinants of Health
If mental health is tied to housing, wages, safety, discrimination, and education, then working on those things is mental health work.
That includes:
- supporting living wages and worker protections,
- backing efforts to create and preserve affordable housing,
- pushing for fair policies in schools, healthcare, and justice systems,
- supporting food banks, mutual aid, and community programs that meet basic needs.
You don’t have to be an expert to matter. Voting, organizing, volunteering, even talking with people in your life about these issues—these are all small but real parts of how society shifts over time.
4. Foster Strong Social Connections and Community Support
And then there’s the quiet, powerful work of simply showing up for each other.
That might look like:
- knowing your neighbors’ names,
- checking in on friends who go silent when they’re overwhelmed,
- joining groups, clubs, or communities where people actually care,
- starting small traditions—regular dinners, walks, or game nights.
Community doesn’t erase mental health challenges, but it changes the experience from “I’m fighting this alone” to “We’re figuring this out together.”

Wrapping It Up: Why Understanding How Society Affects Mental Health Matters
Mental health isn’t just about mindset, motivation, or willpower. It’s about the conditions we’re living in: the cost of living, the safety of our neighborhoods, the stories we’re told about asking for help, the way systems treat us, and whether we have people in our corner.
When we ignore mental health needs, we end up quietly blaming individuals for reacting like human beings to hard situations. We tell people to “self-care” their way out of problems that actually require community care and systemic change.
That doesn’t mean personal choices don’t matter. They do. Therapy can help. Medication can help. Healthy habits and coping skills can help.
But they work best in a world that isn’t constantly working against people.
Understanding the role of society and how it affects a person’s mental well being gives us a bigger, more accurate map. It helps us see that:
- Some struggles are not personal failures, but predictable responses to pressure and inequality.
- Real solutions have to include both individual support and social change.
- We all have some role—small or big—in making things better.
If you’ve been hard on yourself for not “handling things better,” I hope this perspective softens that a little. Maybe it’s not that you’re weak. Maybe you’ve been carrying far more than anyone should have to carry alone.
And if you’re in a place to help—whether that’s listening to a friend, supporting a local organization, or pushing for fairer policies—know that your effort counts. You’re part of the answer to how society affects mental health.
No single article can fix the world. But seeing the bigger picture is a start. Once you can name what’s happening, you’re not just stuck inside it—you’re able to move, choose, connect, and slowly, together with others, change it.





2 Comments
Comments are closed.